I treated chemical attack victims - antidotes should be made available on street corners
29 April is the International Day of Remembrance for all victims of chemical warfare.
There have been more chemical attacks in Syria alone over the last 5 years (60 chemical attacks, 1000 deaths) than the past 70 years combined on the rest of the globe.
As an American Emergency Physician with over 14 years' active duty in the US Air Force and four combat deployments, I have treated a myriad of military and civilian victims including those from chemical weapons.
I have in fact seen and treated virtually every type of war and civilian injury but nothing is quite a jarring as caring for someone burned by chlorine or choked by a toxic gas. Treatment has three objectives: decontamination (remove the agent), antidote (reverse the agent) and supportive care.
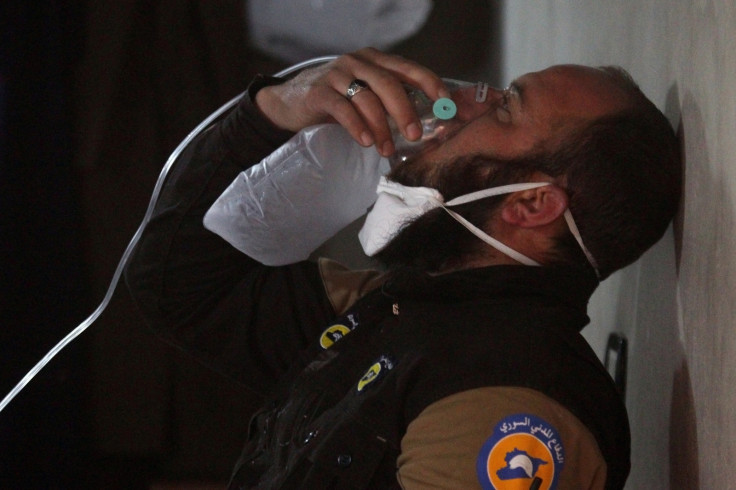
On 4 April 2017 in Khan Sheikhoun, Syria, approximately 600 civilians were injured, 90 died, and thousands of lives were altered by an act of profound cowardice. Many have viewed the videos of children foaming at the mouth, men seizing, and families rushing to a health facility for help. Sarin was confirmed as the primary chemical agent, and some, including me, believe chlorine was likely used as well.
In general, two groups of chemicals are used as weapons – toxic industrial chemicals (TICs) and manufactured chemicals. TICs are common, easily found in large amounts and can be used directly without manufacturing. I treated many US Soldiers and Iraqis injured by chlorine tanks used for water sanitisation but exploded by terrorists.
Manufactured weapons, such as mustard gas and nerve agents (like sarin), are more complex and difficult to manufacture. They require sophisticated engineers, well-trained scientists, and advanced mass production facilities to create even moderate amounts.

The quest to find an antidote
Because of the pressing chemical threat and the immediacy of illness, antidote development must be available to first responders (such as police officers or emergency medical technicians) treating victims on the scene of the attack. Indeed, there is often no time to get a victim to a care facility. While victims of biological agents can be treated with antibiotics, and those exposed to radiation with iodine, no such solution exists with chemical weapons.
For new generation antidotes against chemical weapons to be effective, they must be easily used, stored, deployed and distributed. All weapons of mass destruction are designed to impact many victims, creating a paralysing mass casualty event – their effect is immediate, requiring many to be treated quickly. Drugs administered in the vein through intravenous catheters can take too long and require an advanced skill. They cannot be performed by many first responders or by bystanders. Administering drugs that are ingested, inhaled, or injected rapidly into the muscle is much simpler.
Today, chemicals that do have an antidote are designed to be used by doctors or nurses in hospital Intensive Care Units (ICU) or Emergency Departments, not in the field, where they would have the most impact.
Developers and researchers should adopt a model akin to automated external defibrillators (AED) for cardiac arrest, but for chemical countermeasures – easily available, easily administered, and cost efficient. AED are large boxes found on the walls of airports, schools, and casinos with simple instructions for anyone to use. The same should be expected of antidotes to chemical weapons.
An arduous task
There are many challenges for developing these solutions. Creating medical countermeasures that can be used bystanders and first responders requires small doses that can be injected into the muscle and rapidly absorbed. Often, we do not know what drug a victim has been exposed to, so antidotes must be safe if administered inadvertently. Ideally, the antidote should be inexpensive so it can be widely deployed and useful for treating multiple chemical treats.
Some chemicals such as cyanide, sulfide, or sarin gas are more amenable to antidote development, while others such as chlorine are more difficult. Just like the development of any strategic asset or lifesaving therapy, the timeline for regulatory and funding must be truncated and simplified.
Our team at the University of Colorado in Aurora, Colorado, is working to develop antidotes for civilians against chemical threats, including treatments against cyanide, hydrogen sulfide, and mustard gas with help from academic and industry collaborators across the United States and internationally. Our goal is to bring new simple, effective, and safe antidotes rapidly from the research bench to the patient, specifically designed to be administered easily and simply by almost anyone before the patient reaches the hospital.

Developing medical solutions to counter and treat chemical weapons is not just an academic interest or a general scientific inquiry for me, it is personal. I have lived what most of the world saw on the television on 4 April. I have trained US and international doctors and medics to treat chemical warfare victims, and I have colleagues and friends in harm's way of these threats – as all of us now are.
We need geopolitical solutions to stop their use and medical solutions to save lives. Government agencies, industry partners, and researchers must collaborate in innovative ways to find revolutionary answers.
As we approach the United Nations' Day of Remembrance for all Victims of Chemical Warfare on 29 April 2017, each child and adult who died in Khan Sheikhoun and in every attack before that – as well as those who will inevitably die in future attacks – deserves our attention to rapid development of medical countermeasures and antidotes against chemical weapons.
Vik Bebarta is Professor of Emergency Medicine, Medical Toxicology and Pharmacology at the University of Colorado School of Medicine, Aurora, Colorado, USA.
© Copyright IBTimes 2024. All rights reserved.























