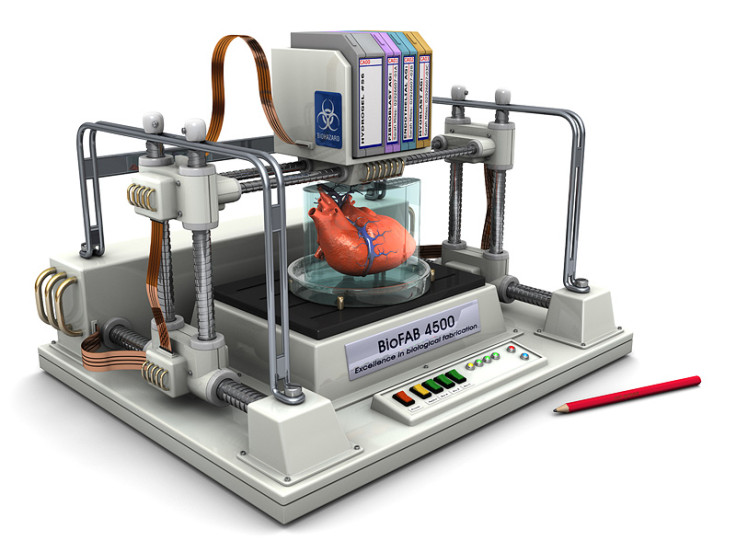
Organovo CEO: 3D bioprinting organs will help us get people off transplant waiting lists
US-based 3D bioprinting firm Organovo has set itself a challenge that could transform the future of medicine, and although the technology is still in its infancy and the challenges complex, the company's founder and CEO Keith Murphy says his firm is in it for the long haul.
"Biotechnology is a very compelling space as you have the ability to impact people's lives," Murphy tells IBTimes UK. "I want to see patients benefiting. We want to help drugs get to patients faster, to get liver tissues [to prolong liver function] and to help people with chronic liver problems."
While 3D printing has been around for over two decades, known in the manufacturing industry as "additive manufacturing" or "rapid prototyping" – a way to produce objects quickly without needing to wait weeks to receive the finished product from a factory in China – 3D printing human tissue is a completely new field.
Murphy was inspired by MIT professor Robert Langer to pursue biotechnology when he was an undergraduate student in biochemistry, and he worked with US biopharmaceutical firm Amgen for a decade before taking a leap into the unknown with bioprinting.
Organovo was born in 2009 and in 2013, the firm started publishing its first results into 3D bioprinting research.
Fast forward to 2015 and it has succeeded in creating 3D printed kidney tissue, while it has several research partnerships with firms like L'Oreal and Merck & Co.
The former wants to take advantage of Organovo's 3D bioprinting technology to develop 3D printed human skin it can test make up and beauty products on, while the latter is keen to test medicine toxicity on 3D printed liver cells, which is a key stumbling block today for getting new drugs to patients quickly.
Organovo was initially privately funded, but from 2012 onwards it has been a publicly traded company. The firm recently undertook a secondary public offering to raise $40m with which to fund its expansion.
Testing out drug toxicity on 3D printed cells
"There are a large number of drugs that have failed in late stage clinical trials, and 30 to 40 drugs have been pulled off the market due to this. For example, there was a drug developed by Warner Lambert and Pfizer called Rezulin [Troglitazone]," says Murphy.
"The drug was developed for diabetes and went on to the market from 1998 to 2000. When it was tested on rats, it was fine. In human trials, there were a few suggestions that there might be live problems, but in human trials, you don't see enough incidents that there's a problem.
"But when it went on to the market, the FDA discovered that it caused acute liver failure in one in every 1,000 patients."
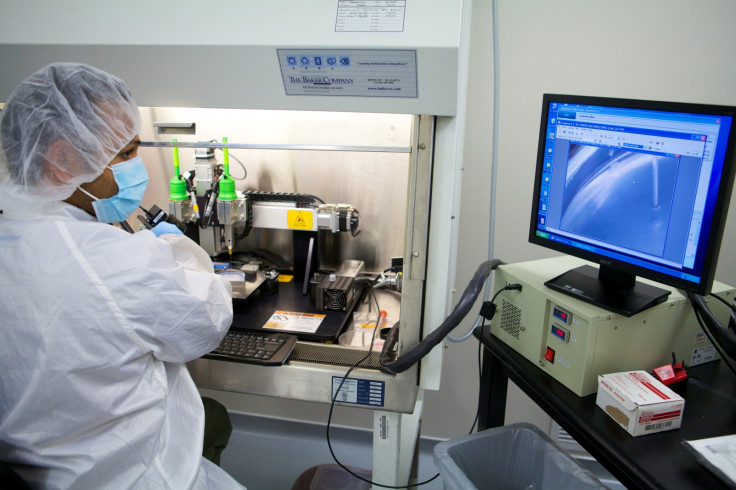
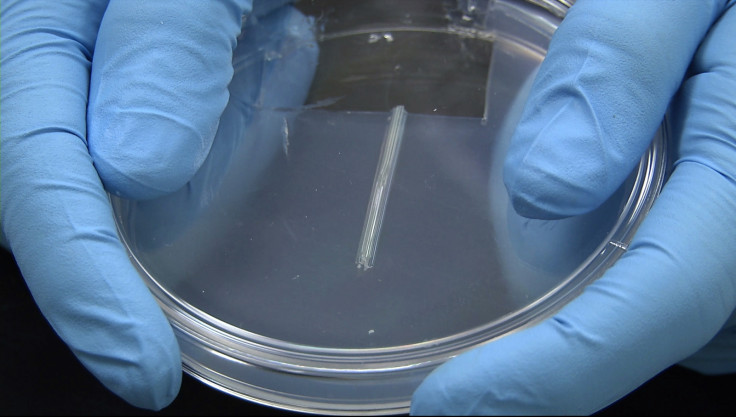
Organovo's liver cells are 3D printed in batches of 24 livers measuring 3mm in diameter and 0.5mm in thickness. Each batch takes 45 minutes to print.
Murphy says Organovo tested Rezulin on its 3D printed liver cells and within seven days, the drug caused significant damage to the cells.
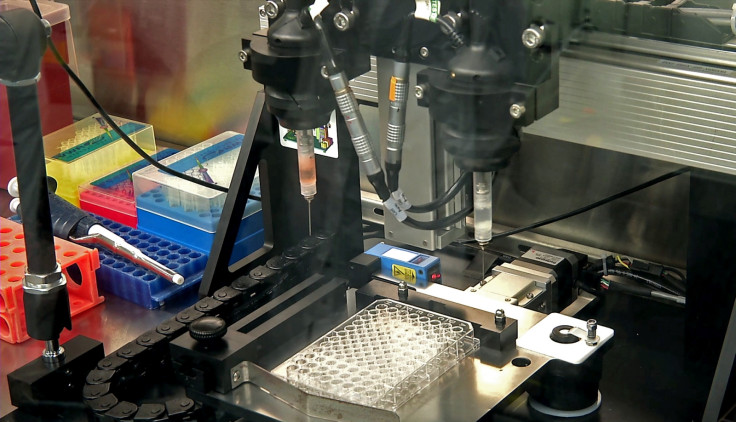
This is one of the key uses that 3D printed cells could serve, as there is only so much you can do with laboratory-grown cells, since cells behave differently in the body, compared to cells grown on a petri dish.
"First of all, we've got to penetrate the existing market for this, get these tissues to more pharma companies. We are currently marketing 3D printed livers, while the kidney will be launched in September 2016," says Murphy.
"Longer term, we want to continue developing tissues for drug discovery with partnerships. We're testing right now in a number of early stage preclinical studies for a number of tissues that we expect to get into trials."
But 3D printing organs is where the true dream lies
In particular, Murphy sees being able to test drugs for Alzheimer's disease as a key benefit of testing drugs on 3D printed cells, as the drugs would be able to make it to the market faster and be able to halt brain degeneration.
However, he is most excited about being able to 3D print entire human organs, although there are still many scientific and technical hurdles ahead.
"The biggest challenge to making larger tissues is keeping them alive. We could print a larger block of tissue but it wouldn't survive because the cells need oxygen and nutrients. You need a full vascular system like the one that exists in the body to keep those cells alive," says Murphy.
The tissue people make today are quite limited in size. What people can't make yet, is that vascular tree inside of living tissue
"If you were to transplant an organ, the key thing you would have to do would be to take an artery that's attached to the organ and attach it to an artery in the body as a source of blood supply.
"The tissue people make today are quite limited in size. What people can't make yet, is that vascular tree inside of living tissue."
In the past there have been ethical and moral objections to the science of cloning, particularly from religious organisations, and Gartner predicted in 2014 that by 2016, governments could be debating whether to ban the technology.
"I don't see it being controversial to help solve problems. Of course you need FDA and MEA overseeing the process, but I don't see a problem. A long time ago people were resistant to using cadavers, but it's clear now that there's so much you can gain from using them in research, that now it's not controversial at all. I think this will happen with 3D bioprinting as well," Murphy argues.
"Yes we're using it for toxicity, but you could use it to build a vaccine to protect against Hepatitis C getting into the liver, and then there's genome sequencing. We see our technology as a platform with a large growing number of applications.
"I've got loved ones on transplant waiting lists and loved ones affected by certain diseases, and so do my colleagues. It's something that motivates our entire staff."
© Copyright IBTimes 2025. All rights reserved.