Does HIV treatment increase the risk of unprotected sex – and syphilis?
Among men who have sex with men, the risk of getting syphilis is increasing, and HAART could be a factor.
HIV treatment could increase people's susceptibility to developing another sexually transmitted infection, syphilis. Highly active antiretroviral therapy (HAART) could indeed deregulate the body's immune response to the bacteria that causes syphilis.
Introducing HAART has been a turning point in the fight against HIV and Aids. The drugs, which are now taken by millions globally, successfully reduce the risk of the virus developing resistance, decrease mortality rates, and improve HIV patients' quality of life.
Since the turn of the century, it is estimated that the number of new infections fell by 35% and Aids-related death by 28% – alongside prevention, the distribution of antiretroviral therapy was key to this success.
However, the fact that HAART is so effective has led to unexpected problems. Many people have started to believe that transmission is now much less likely and that getting infected with HIV is not a death sentence anymore. As a result sexual risk-taking is believed to be on the rise.
This is particularly the case among men who have sex with men, with many engaging in unprotected sex. This leaves them vulnerable to other sexually transmitted diseases and data shows that there has been a rapidly escalating outbreak of chlamydia, gonorrhoea and infectious syphilis in this group in recent years.
However, among men already infected with HIV, the rate of syphilis infection has grown more rapidly than that of other sexually transmitted infections, leading scientists to investigate whether HIV treatments could increase people's susceptibility to the disease.
Bacteria Treponema pallidum
The team, led by Dr Michael Rekart from the University of British Columbia, reviewed scientific literature to analyse the impact of HAART on behavioural and immune system changes. The data they collected enabled them to create risk models to assess the likelihood of syphilis infection – in which people taking HAART were predicted to have more sexual partners and to have greater susceptibility to Treponema pallidum, the bacteria responsible for syphilis.
The models suggest that both factors combined – having a greater number of partners and a greater susceptibility to the bacteria – produced a peak in the number of infections that was greater than that associated with either factor alone.
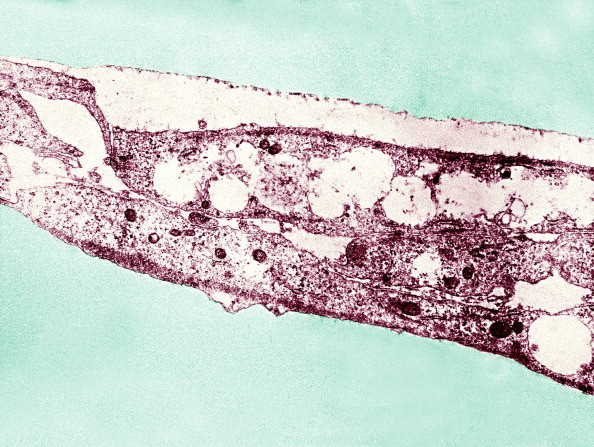
The scientists also came up with an explanation as to why HAART increases susceptibility to Treponema pallidum. Reviewing biological evidence available in past research, they say that active antiretroviral therapy may alter the innate and acquired immune responses in ways that enhance susceptibility to Treponema pallidum. This heightened susceptibility could be a major factor in the rising incidence of syphilis in HIV-positive men who have sex with men.
The complete findings are now published in the BMJ.
A number of limitations
The study provides new ways to consider the rising number of syphilis infections, but it does not in any way suggest that people should stop taking HAART. Instead, the focus should be on prevention and on explaining that these drugs do not stop other sexually transmitted diseases.
A number of limitations to the study can be highlighted. In an editorial, three scientists have warned that the reason why syphilis cases appear to be more prevalent than other sexually transmitted infections is that gonorrhoea and chlamydia are often asymptomatic, and most cases are often missed because extragenital testing is not performed.

Additionally, the models greatly simplify reality. Taking HAART does not necessarily increase the number of sexual partners and does not look at couples' dynamics in sufficient details. "They assume that all partnerships have the same level of syphilis risk, whereas the reality may be more complicated... They model increased behavioural risk through increasing number of partnerships, but do not capture other aspects of transmission risk, such as decreased use of condoms within partnerships", the scientists note.
Likewise, they do not include in the models how being at a different stages of an HIV infection influences the risk of getting syphilis.
However, the findings are interesting because they remind health professionals that effectively treating and preventing HIV should not limit their efforts to control other sexually transmitted infections.
© Copyright IBTimes 2025. All rights reserved.






















