E.coli 2011 outbreak: Over-use of antibiotics may have created new strain
The E.coli outbreak sweeping Europe is the deadliest on record: 22 people have died and there have been over 2,000 reported cases in nine countries.
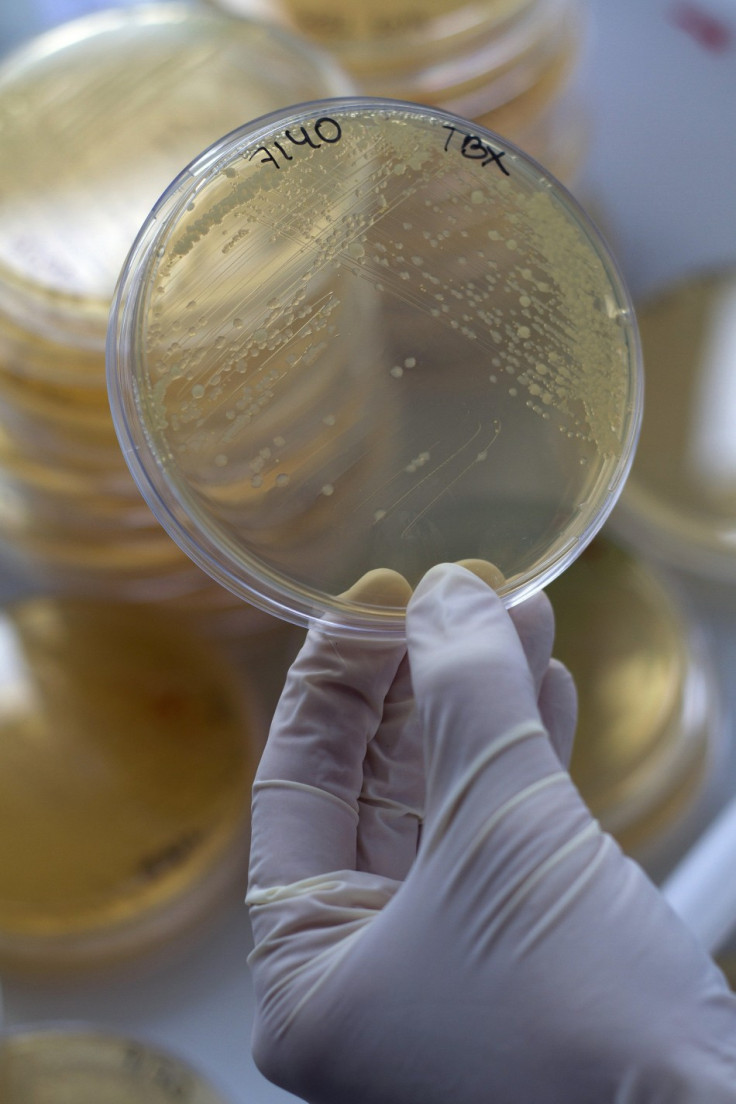
Ordinarily, E.coli is a harmless bacteria found in the gut. They are found in every other mammal, too. Just like us, the bacteria have sex and get old. They send out assassins. They form biofilms that resemble cities.
But in the mid-1900s, scientists began uncovering strains of E.coli that could cause life-threatening diarrhea. Unlike ordinary E.coli, they carried genes for a poison known as Shiga toxin, named for Japanese bacteriologist Kiyoshi Shiga. Over time, microbiologists identified a number of strains of disease-causing bacteria, classifying them by the proteins on their surface.
It is one of these strains that have caused the current outbreak in Germany. It enters the food chain via contamination with faecal material.
As health official struggle to trace the outbreak to a food that can be removed from the market, it has focused international attention on the complex paths that have led to the emergence of this rare strain of the bacteria.
New Strain
On 2 June, Chinese researchers reported that the strain involved in the German outbreak was not the E.coli that caused similar previous outbreaks, known as O157:H7. In fact, it was an entirely different strain, called O104:H4, that had never been associated with epidemics before.
According to Newsweek, Phillip Tarr, a microbiologist at Washington University, searched the medical literature for reports of the European strain. He only found a handful of people who had carried it, and none of them fell ill. Somehow this rare microbe had turned deadly, triggering the biggest E. coli epidemic in history, with at least 2,000 infections and 22 deaths (at time of writing).
"We didn't know this bug was out there," says Tarr. "This outbreak is taking us all by surprise."
Modern food systems
Modern food production can spread the bacteria far faster than ever before. In 2006, for example, E. coli on contaminated spinach infected 199 people in the United States, causing kidney failure in a number of cases. But of most concern was that the outbreak swept across the country before public-health workers became aware of it.
The UK's worst E.coli outbreak to date, in Lanarkshire in 1996, killed 21 people. The source -- a small butcher's shop where there was cross-contamination between raw and ready-to-eat meats -- was fairly quickly identified because the cases were localised.
In contrast, although the current outbreak of E coli appears to affect people in northern Germany, or those who have been there, the source of the poisoning is shrouded in mystery. The key difference here is that the Lanarkshire people were eating local meat. Whereas, in Germany and the USA, consumers were eating salads that came from hundreds of miles away, making it much harder to pinpoint the source.
A recently published report found that more than 99 per cent of the produce grown in Santa Barbara County, California, is exported, and more than 95 per cent of the produce consumed in the county is imported, some of it from as far away as Chile, Argentina, and New Zealand.
The E.coli outbreak in 2006 was eventually traced to a wild boar that may have carried the bug in from a nearby cattle farm. Industrial farming means that even those on a vegan diet may reap the nastier effects of intensive meat production. It is no longer enough for individuals to switch to "healthier" choices in the supermarket.
As modern food systems increasingly rely on produce grown and shipped from far-flung countries the potential for similar outbreaks to spread increases. And the difficulty in tracing the sources of contaminated food is all too evident.
Deadly Evolution
A look at the genetic makeup of E.coli O157:H7 (the closest relative to the current outbreak that has been studied in any depth) is cause for even more concern. Newsweek reports it evolved into a deadly pathogen by picking up genes from other bacteria through a process called recombination. Viruses, for example, can move from one E.coli to another and insert genes from their old host into a new one.
"E.coli are a cauldron of recombination," says microbiologist Phillip Tarr.
Health officals have been surprised by the new strain's emergence because the current variation does not belong to any well-known suspects.
Initially, it appeared that the bacteria were coming from cucumbers and other vegetables from organic farms in Spain, but O104:H4 has not turned up in tests at those places.
The current bacteria's genome sequence suggests that it's yet another concoction entirely. The bacteria contain many segments of DNA not seen in other E.coli strains. This new DNA may be responsible for its high level of toxicity -- more than a quarter of victims have gone on to develop the dangerous form of the disease. Of greater concern is that the O104:H4 strain has acquired new genes that make them resistant to antibiotics. As a result, doctors have few options to treat the bacteria. In Germany, physicians are resorting to an experimental antibody treatment to see if it can help.
Uncharacteristic Evolution
It is the strain's resistance to multiple antibiotics that has caused most unease amongst health officials. Privately, many scientists are concerned that the vast overuse of antibiotics throughout the food chain has created this deadly outbreak.
O104's resistance profile has been briefly in media reports, but this is a curiosity that distinguishes the strain rather than a concern. That is largely because the safest way to treat infections caused by an E.coli strain that also produces toxins, as this one does, is to refrain from using antibiotics - since when the drugs kill the bacteria, they cause the toxins to be released and bring on the illness's worst symptoms.
The significant antibiotic resistance has raised alarm bells because Shiga-toxin producing E.coli strains such as O104:H4 and O157:H7 are rarely resistant - this means that new defences have been acquired from elsewhere.
"Their presence in this new strain demonstrates how freely resistance factors can jump among organisms once they emerge. And that should underline how important it is to slow down the evolution of antibiotic resistance, by cutting back inappropriate use of antibiotics in everyday medicine and on farms," science journalist Maryn McKenna said.
Misuse of Antibiotics
Where are these resistance factors coming from? As the Guardian reports, the development of resistance is an inevitable biological process; it's what bacteria do to protect themselves against deadly compounds, whether the compounds were made naturally by other bacteria or artificially in a drug-development lab. But excessive exposure to antibiotics accelerates the process and makes its results unpredictable.
That excessive exposure happens any time anyone takes antibiotics for a health problem for which they are inappropriate, such as colds or ear infections. It happens even more when low-dose antibiotics are deployed extensively in large-scale agriculture, without any oversight to report back what antibiotic-resistant strains are emerging.
Currently, more antibiotics are now being fed to animals - to promote growth - in North Carolina than are given to the entire human population in the United States.
This outbreak should be a warning call for the deadly spread of resistant microbes. Given bacteria's unrestrained potential to exchange genetic material, we know that O104 is keeping that resistance going by harbouring it and handing it off to yet another species.
If there's something to take away from the German outbreak it is convincing governments and health authorities to do what they can to slow down the evolution of drug resistance, by curbing the antibiotic misuse that brings it into the world.
© Copyright IBTimes 2025. All rights reserved.





















