World Cancer Day 2015: Terminally ill cancer patient cured by miracle drug Ipilimumab

KEY POINTS
- Drug trial helped cure patient who was told to put his affairs in order after chemotherapy failed
- Medical professionals should establish difference in patient having incurable disease vs terminally ill
Recently, former health minister Lord Darzi criticised the NHS for wasting money unnecessarily on treating terminally ill cancer patients, arguing that the money should be saved and put towards new drugs and treatment techniques instead.
His comments came on the back of plans to cut David Cameron's Cancer Drugs Fund, which could see over 50% of current drugs cut and has had the pharmaceutical industry up in arms.
There are two sides to the coin with this argument – on one hand, cancer drugs are expensive and cuts must be made somewhere in order for new treatments to be brought in, but on the other, are people who have been labelled as "terminally ill" truly out of our reach to treat?
Morgan Giles, 71, is living proof that fighting back against cancer is possible, having recovered almost completely from stage four malignant melanoma – the most dangerous form of skin cancer.
The retired grandfather from Yeovil, Somerset had previously worked in Saudi Arabia as an aircraft welding teacher for eight years, and hadn't really thought much about skin cancer until doctors found a cancerous mole on his shoulder in 2006.
After it was removed, Giles felt fine for five years, but then in 2010, doctors discovered that the skin cancer had spread through his body, and he now had five brain tumours, as well as dozens of tumours on his lungs and abdomen.
Unfortunately, several rounds of chemotherapy failed to have any impact on the tumours, and Giles was told by specialist doctors to put his affairs in order in 2011.
However a friend he hadn't seen in 30 years who lived in the US contacted him out of the blue and told him about a cancer trial his son was working on.
In the end, Giles couldn't be accepted to the trial as he wasn't a US citizen, but when he spoke to his local GP, the doctor found out about a similar trial happening at Royal Marsden Hospital in London and sent his information through.
Ipilimumab: Destroyer of cancer cells

Ipilimumab, under the brand name Yervoy, is an immunotherapy, i.e. a drug that alters the immune system to see tumours as foreign, which then destroys them.
Even though all the medication for the trial had already been allocated to participants, the head of the trial, Professor Martin Gore, made a special request to get some more for Giles on compassionate grounds.
"Initially I had a mixed response to the drug for six months, but the tumours began shrinking immediately. It took 2.5 years for the tumours to die or become dormant and now thankfully I'm as right as rain," Giles tells IBTimes UK.
"We don't know if it's going to come back, but they've said everything is gone. When I asked to see the tumours on the computer screen, there was nothing there."
Professor Gore says that until fairly recently, the outlook for patients with malignant melanoma has been bad with "really no affective treatments at all", and although Ipilimumab has been touted as a wonder cure, in reality the drugs do not work on everyone.
"[Morgan] was treated at a time when there was an indication that this drug would make a big difference. He is one of those 20% of patients who will have a long-term benefit or even cure from this disease," Gore tells IBTimes UK.
"We are trying to identify the people who will benefit from these types of treatment and the people who won't. I think the result with Morgan is particularly gratifying.
"There were some features of his disease that worried us about whether Ipilimumab would work. It's such a wonderful result because our fears have been proven wrong."
Ipilimumab also works with another family of drugs known as anti-PD1 and Royal Marsden Hospital, like many other medical institutions around the world, is now working to combine the two drugs together in order to shrink the tumours and produce even better results, but these are still undergoing trials.
"There's been targeted agents, and for those [patients] that have the right mutations in the tumours, you can get a very high rate of success in shrinking the tumour, but it gradually builds up a resistance. They're used routinely, but they're not the answer. They are helpful, but we can do better," he says.
Efforts should be made to exhaust all possible treatments
In regards to Lord Darzi's comments, Gore believes that it is important for medical professionals to be able to distinguish the difference between terminally ill patients, and patients who have a condition that is not curable.
"The term 'terminally ill' means someone is actively dying, which is not the same thing as having a condition where there is no hope of long term survival," he says.
"If someone is dying and nothing can help them, then they shouldn't be given that treatment. But if there is something that can be done to help them, the treatment should be discussed by the doctor with them and their family."
Gore believes that cancer treatments that have been shown to be effective should be funded.
"I don't think with cancer treatments it's a competition between different types of cancer, the message for cancer is that early diagnosis and effective treatment, whatever treatment, is all important," he says.
While Yervoy is now available on the NHS, if doctors like Gore hadn't believed that Giles could get better, things could have turned out much differently.
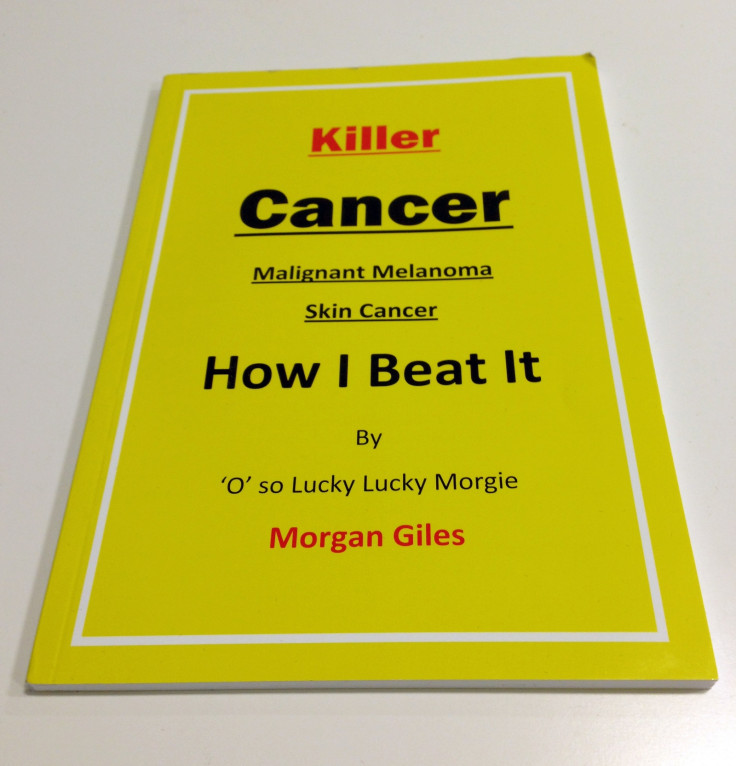
Giles is so thankful and relieved to have survived cancer that he has written a book entitled "Killer Cancer Malignant Melanoma Skin Cancer: How I Beat It" – a diary that details the four years of his cancer treatment, and how he felt through the ups and downs, which can be ordered by emailing morganwgiles@gmail.com.
He has also detailed some visualisation exercises and his personal journey of believing that he would get better.
He has so far sold 300 copies and all proceeds go to St Margret's Hospice, his local hospice, with the long-term goal of funding further cancer research at Royal Marsden Hospital.
"Why have I got away with it and so many people have not?" he asks. "I believe in what I've been doing. Believing is what helps you survive."
© Copyright IBTimes 2025. All rights reserved.






















