Aids epidemic no longer a public health issue in Australia, but HIV still is
Australia's 'end of Aids' boast is great, but there are still huge obstacles to overcome.

Jennifer Power, La Trobe University
Aids is no longer a public health problem in Australia. This is the announcement that came earlier this week from leading scientists at the Kirby and Peter Doherty institutes and the Australian Federation of Aids Organisations (AFAO).
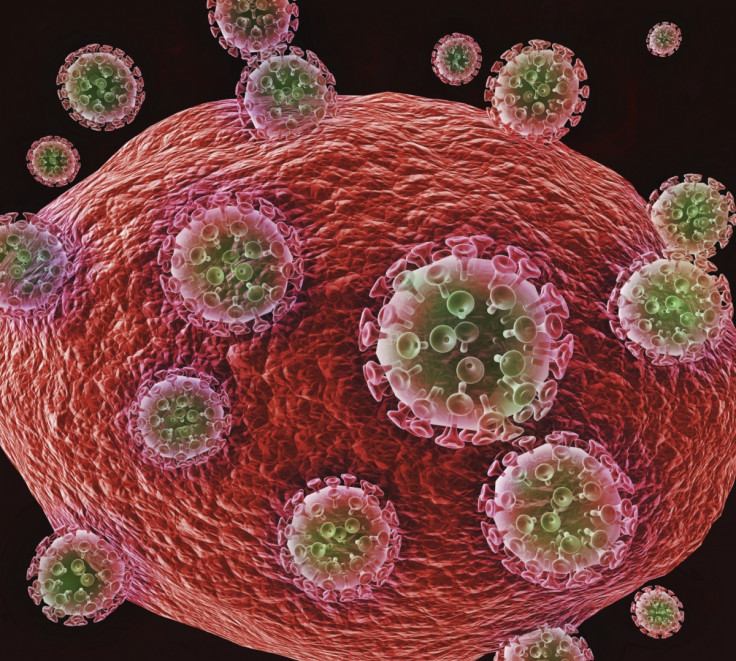
But what does this really mean? Aids is the syndrome caused by damage to the body's immune system that results from HIV. Aids is an advanced stage of HIV infection, occurring when the body no longer has capacity to fight off infections and other illnesses.
However, modern antiretroviral treatment (ART) is so effective at suppressing HIV within a person's body, that people consistently using ART are unlikely to ever develop Aids.
ART is a lifelong treatment regimen for people living with HIV. If ART is stopped, HIV will rapidly rebound in the body, causing damage to the immune system and increasing the likelihood that the virus can be transmitted to others.
The most recent national HIV surveillance data estimated that 73% of Australians living with HIV are currently using ART. Other research has suggested this figure may be even higher.
Given widespread use of ART in Australia, cases of Aids are so few that they are no longer recorded on public health registers.
This is a major achievement. Since 1982, more than 35,000 Australians have been diagnosed with HIV and around 10,000 have died from Aids-related illnesses. At the epidemic's peak in the mid-1990s, there were close to 1,000 new diagnoses of Aids each year – the majority among men in their 20s and 30s.
That Australia can now boast the "end of Aids" is testament to the internationally recognised success of Australia's response to HIV and Aids – which has incorporated community, clinical and bio-medical responses to HIV prevention, testing, treatment and care.
But Aids is different to HIV. While we may not see many cases of Aids in Australia today, HIV is very much an important public health issue in this country.
There are currently more than 27,000 people living with HIV in Australia and around 1,000 new cases are diagnosed each year.
People living with HIV still require specialised clinical and support services, especially as people age and need to manage HIV alongside other chronic conditions.
HIV prevention is increasingly complex in Australia today. While the majority of new HIV infections still occur among men who have sex with men, we are seeing increasing new diagnoses among Indigenous Australians as well as migrant communities and mobile populations such as transient workers.
Alongside this, HIV prevention initiatives need to adapt to the introduction of new bio-medical prevention technologies such as pre-exposure prophylaxis. Without a sophisticated and flexible approach to HIV prevention, Australia will not be in a position to reduce the current rate of new HIV diagnoses.
Overlaying all of this is the reality that HIV, unlike most other chronic illnesses, is still imbued with widespread stigma, discrimination and misunderstanding.
The psychological and social impact of HIV stigma negatively affects the health and well-being of many people living with HIV in Australia.
One of the benefits to highlighting the end of Aids is that it draws public attention to the reality of HIV today and how different it is to the 1980s or 90s when Aids was more prevalent. Most Australians who contract HIV today will never get Aids. If people have an undetectable amount of HIV in their system, which is often the case among people using ART, they have almost zero chance of transmitting HIV to others.
Much of the discussion and imagery associated with Aids and Aids-related illnesses perpetuates the association between HIV, illness and death. This increases stigma, which in turn creates more barriers to HIV prevention, testing and care. So it makes sense to divorce HIV from Aids in Australia.

But it would not make sense for many other countries. Calling out Australia's success in curtailing Aids provides a platform to draw attention to other countries where Aids is still a major public health problem.
Globally, more than 35 million people live with HIV, most of whom live in countries where ART is not readily available or affordable. In 2014 alone, more than 1.2 million people died from Aids-related illnesses.
If Australia can show that it's technically feasible to "end Aids", we can see that not achieving this in other countries is a problem of lack of resources and, in some cases, lack of political will, which is often associated with stigma.
Researchers at the Kirby and Peter Doherty institutes, along with AFAO, linked their announcement about the end of Aids to a call for Australia to increase funding to the Global Fund to tackle HIV in the Asia Pacific Region where more than 200,000 people die from Aids-related illnesses each year.
So there are good reasons for drawing attention to "the end of Aids" in Australia. But this needs to be read with caution. This is not a call to change Australia's approach to HIV prevention, treatment and care. If anything, it points to the importance of continuing Australia's strong public health response to HIV and for the Australian government to support a global "end" to both HIV and Aids.
Jennifer Power, Senior Research Fellow at Australian Research Centre in Sex, Health and Society, La Trobe University, La Trobe University
This article was originally published on The Conversation. Read the original article.
© Copyright IBTimes 2025. All rights reserved.





















