Alzheimer's: Landmark study unravels secrets of how brain cells degenerate
The research could have huge implications for treating and preventing the disease.
A new study has untangled the process by which brain cells in Alzheimer's patients degenerate, a mystery which scientists have not been able to explain fully till now. The team from the University of North Carolina School of Medicine (UNC) believe the findings will open up new avenues of research into how to treat and prevent the disease.
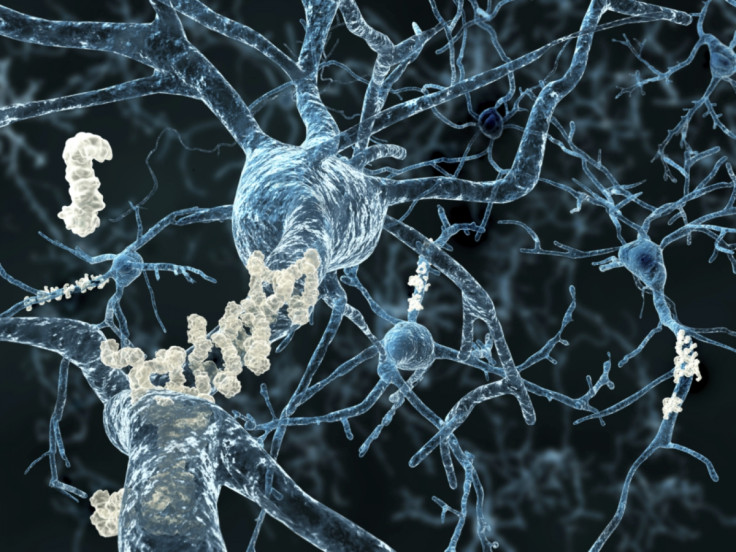
In the brains of people with the disease, three seemingly separate phenomena can be observed. Firstly, there are abnormal amounts of two different proteins – called amyloid beta and tau. As well as this, the brain's immune cells –which protect the body against infectious disease and foreign invaders - are usually found in an activated state. But scientists have struggled to understand how these three contributing factors combine to drive the disease.
However, the UNC team have established a link between the three elements by examining lab-grown human cell cultures which were designed to mimic conditions in the brain. They found that the amyloid beta proteins created a striking inflammatory response in the body's immune cells which in turn can damage neurons – the cells that transmit electrical impulses in the brain.
Following this realisation, they were able to show how this kind of neuron damage led to the formation of abnormal swellings resembling a string of beads. These formations were filled with the tau protein. Bead-like structures such as these are often found in the brains of Alzheimer's patients.
This 'beading' process, as it is known, has been observed in Alzheimer's patients and has been considered an early sign of brain damage. However, up until now, the link between tau proteins and 'beading' was unclear. Scientists were also not certain if 'beading' necessarily led to Alzheimer's disease.
"It's exciting that we were able to observe tau - the major Alzheimer's protein - inside these beaded structures," said Todd Cohen, an assistant professor of neurology. "We think that preventing these structures from forming would leave people with healthier neurons that are more resistant to Alzheimer's."
Finally, the researchers identified the important role of two more proteins – called MMP-9 and HDAC6 respectively – which act as a catalyst, creating the perfect conditions for these interconnected processes to occur. They are also found in high concentrations in the brains of Alzheimer's patients.
The implications of this are important because now that these two crucial proteins have been identified, they could be targeted by new drugs which could treat or even prevent Alzheimer's. In fact, drug companies are currently developing and testing HDAC6 inhibitors which work by limiting the effects of this protein. These drugs have performed surprisingly well in early studies but scientists have not fully understood the mechanisms by which they were working.
"Our work might explain why HDAC6 inhibitors have shown such early promise," Cohen adds.
Furthermore, treatments focused on blocking the effects of MMP-9 and HDAC6 could also prove useful elsewhere. This is because the creation of the bead-like structures seen in the experiment is also seen in various other neurodegenerative conditions, as well as head injuries. This 'beading' has even been detected on a small scale in otherwise healthy elderly brains. Indeed, Cohen suggests that it might be one of the processes that contributes to general cognitive decline.
© Copyright IBTimes 2025. All rights reserved.





















