Cervical cancer screening: A step-by-step guide to getting your smear test
A third of young women avoid cervical screenings because they are embarrassed by their genitals.
Cervical cancer is the most common cancer in women under 35, but a third of young women avoid getting screenings because they are embarrassed by their genitals.
That's the shocking truth according to a survey of over 2,000 women in the UK by the charity Jo's Cervical Cancer Trust, which also showed that almost two-thirds of women aged under 35 were not aware they were the most at risk age group.
Cervical cancer is the second most common type of the condition in women worldwide. It claims over 800 lives in the UK each year, according to Cancer Research UK. The cervix is the lower part of the uterus. It helps menstrual blood flow from the vagina and acts as a passage for sperm to enter during sex.
Women between the ages of 25 to 49 are advised by the NHS to have a cervical screening every three years, dropping to five years for those aged 50 to 64. Only women with abnormalities in the past need tests after the age of 65.
A woman who didn't have a smear test until the age of 30 told BBC News she put it off because she was "naive, embarrassed and uneducated about the female body".
Lauren Bennie, 33, from Glasgow told the website that she was worried the nurse would be able to "take one look at my bits and have some magic skill to be able to determine the number of sexual partners I'd had".
Jo's Cancer Charity is urging women to attend potentially life-saving smear tests, marking Cervical Cancer Prevention Week from 22 to 28 January.
So what exactly happens during a cervical screening?
First, a medical professional such as a nurse, doctor or gynaecologist will take the patient into a private room, ensuring the door is locked. Patients are asked to remove the bottom half of their clothing, including underwear, and place their feet in stirrups to provide access to the genital area. A large piece of tissue can be used to cover the pubic area.
A medical tool called a 'speculum' is then used to gently widen the vagina. A plastic speculum is most commonly used, although some clinicians may use metal ones. Sometimes a clinician may put lubricant on the device so it is easier to insert into the vagina.
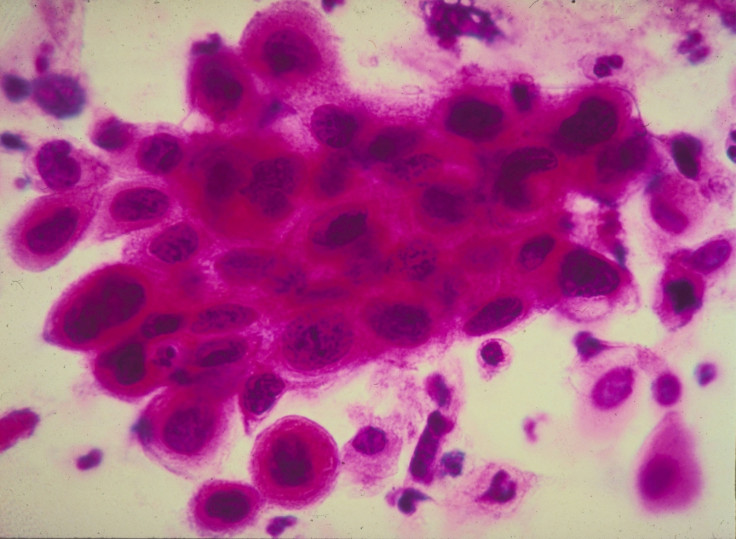
A spatula or brush, thinner than a pencil, is then inserted into the opening of the cervix, and rotated in order to collect cells. These are then preserved in a liquid container or on a glass slide, and sent off to a lab for testing. The speculum is then removed and the test is over. A cervical screening takes around three minutes, according to Jo's Cervical Cancer Trust. An appointment will generally last no more than 20 minutes.
If the sample shows low-grade or borderline cell abnormalities, a doctor may recommend that a patient undergoes a colposcopy: a procedure which can confirm if they require treatment to remove the cells at a later date.
"People might feel exposed or embarrassed during pelvic exams, but they should not be painful," Nicole Telfer, a scientific researcher at the female health app Clue, told IBTimes UK.
"None of the parts of a pelvic exam — which includes testing for HPV and cervical cancer — should elicit pain in a healthy person."
She added that the procedure is ""not painful, but it may feel strange or slightly uncomfortable.
"This makes sense: your cervix is located in a place that is not usually touched in isolation. In my personal opinion, the weirdest part of getting a pelvic exam is just the presence of air flow into my vagina — this seems the most uncomfortable to me.
"If if you do feel any pain, tell your healthcare provider," she added. "These exams are necessary to assess your genital and reproductive health."






















