COVID vaccines work well for people of all body weights – but underweight and obesity remain risk factors for severe disease

Since the pandemic began, more than 6 million people have died from COVID around the world. The good news is that we now have a wide range of treatments as well as highly effective vaccines which have helped reduce the number of severe COVID cases.
Still, some people are more likely to get very sick or die from COVID than others. Our research, carried out before vaccines became available, showed that obesity is one of the factors that increases a person's risk of being hospitalised or dying from COVID. We have now followed this up with a new study looking at how body weight affects the uptake and effectiveness of COVID vaccines, and discovered that being underweight can also be a risk factor for severe disease.
Obesity is measured using the body mass index (BMI). This is calculated by dividing a person's weight in kilograms by their height in meters, squared. A person with a BMI below 18.5 is considered underweight, in the range of 18.5–25 is considered healthy weight, above 25 is considered to be overweight, and above 30 is considered obese.
These early findings on the people most at risk were used to support policies that prioritised certain groups of people for vaccination. This included people with a BMI of 40 or above.
Other research from before the COVID pandemic has shown that people with obesity are less likely to take up seasonal flu vaccines. There's also evidence to suggest that some vaccines work less well in people with obesity, although we don't fully understand the reasons for this.
What we did
In our new study, published in The Lancet Diabetes & Endocrinology, we used anonymous health records from more than 9 million people aged 18 and older in England. Our data covered the period from December 8 2020 (the date the first COVID vaccine was administered in the UK) until November 17 2021. During this time, 566,461 people out of the 9 million tested positive for COVID, of which 32,808 were admitted to hospital and 14,389 died.
To investigate vaccine effectiveness across different body weights, we looked at the risk of severe COVID outcomes (such as hospitalisation and death) across the full BMI range. Within BMI groups, we compared people who were vaccinated with people of the same age, sex and other characteristics who hadn't been vaccinated.
We found COVID vaccines were highly effective against severe outcomes in all BMI categories, especially after the second and third doses. After the second dose, vaccinated people in healthy weight, overweight or obesity groups were almost 70% less likely to be hospitalised as a result of COVID than their unvaccinated counterparts. Similarly, vaccinated people in the healthy weight, overweight and obesity groups were around 60%–74% less likely to die from COVID than unvaccinated people with the same BMI.
Read more: COVID vaccines for children under five: what parents need to know
Our results indicate that COVID vaccines may be slightly less effective in people who are underweight. Vaccinated people who were underweight were around 50% less likely to be hospitalised and around 40% less likely to die than their unvaccinated counterparts. Of course, this still represents a good level of protection.
People who were underweight were also the least likely to get vaccinated in the first instance, and this was true across all age groups. The proportion of fully vaccinated people was highest among people who were overweight and obese. In our study, fully vaccinated meant having received two or three doses, as not everyone was eligible yet for a booster at the end of our study period.
Uptake of vaccination by age and BMI
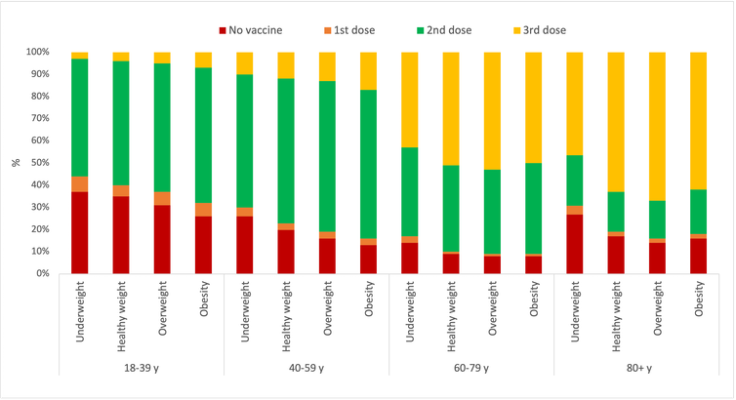
We also looked at the risk of severe COVID outcomes only among the people who had been vaccinated with at least one dose. Although vaccination massively reduced the likelihood of severe COVID, people who were underweight and those with obesity remained at greater risk of hospitalisation or death from COVID than people of a healthy weight. This was also the case before vaccines were rolled out.
Risk of COVID hospitalisation and death after two vaccine doses by BMI
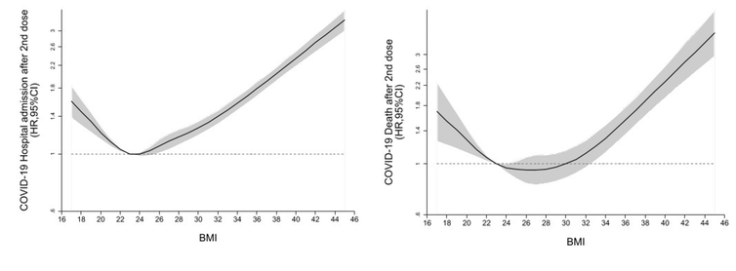
The associations became less significant among those who had received a third dose. But as only a limited number of people were eligible for the third dose by the end of the study period, we'll need further research to better understand the effect of boosters.
The data also didn't allow us to explore any differences between the different COVID vaccines, or to assess the influence of different COVID variants.
Read more: Inflammation: the key factor that explains vulnerability to severe COVID
People who have two doses of a COVID vaccine receive a high level of protection against severe outcomes, regardless of their body weight. Given the slight reduction in vaccine effectiveness in people who are underweight, targeted efforts may be needed in this group to increase vaccine uptake.
Even though severe outcomes were much rarer after vaccination, people in the underweight and obese groups were at significantly higher risk compared to people of a healthy weight.
Public health strategies to help people achieve and maintain a healthy weight have many benefits. One important one may be to help reduce the burden of severe COVID.
Nerys M Astbury currently receives funding from NIHR Biomedical Research Centre Oxford, NIHR School of Primary Care Research, Diabetes Research and Wellness Foundation & Diabetes UK and is currently elected as a trustee of the Association for the Study of Obesity (ASO).
Carmen Piernas received funding from the NIHR Applied Research Collaborations - Oxford (UK) during the conduct of this study. She is currently a Ramon y Cajal fellow at the University of Granada (Spain), funded by the Spanish State Plan for Scientific and Technical Research and Innovation 2017-2020 (RYC2020-028818-I). This study was supported by Health Data Research UK (HDRUK) in partnership with the Office for National Statistics and funded by UK Research and Innovation. It was also supported by the NIHR Oxford Biomedical Research Centre (BRC) and the NIHR Oxford and Thames Valley Applied Research Collaboration.





















