Opening patient's skull after traumatic brain injury reduces risk of death
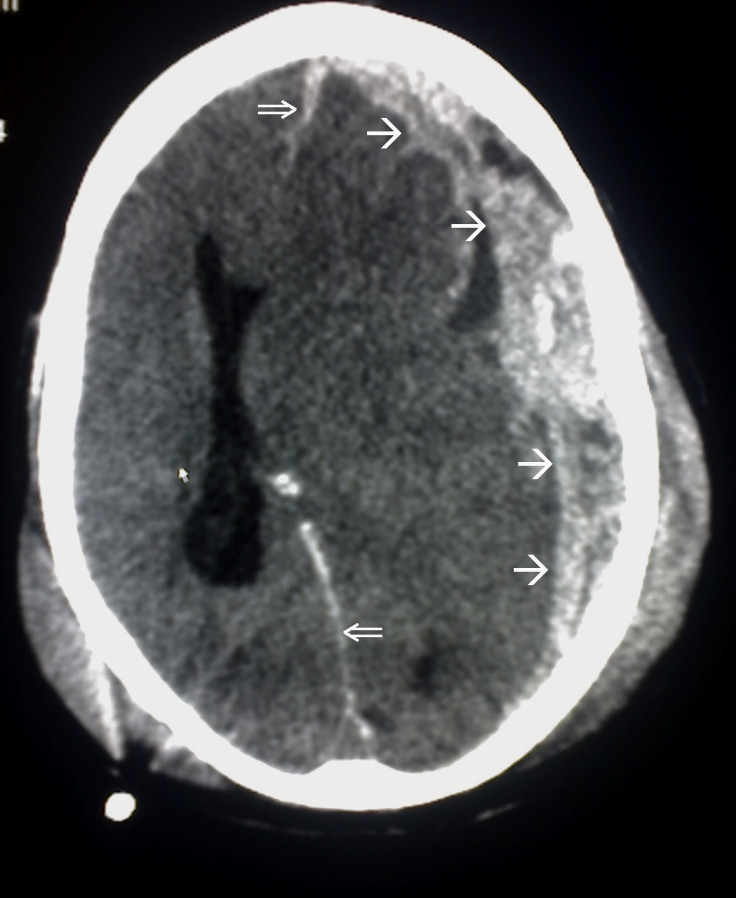
Craniectomy involves the surgical removal of parts of the patient's skull.
Traumatic brain injuries, which often occur as a result of road accidents, assaults or falls, can lead to dangerous swelling in the brain, which in turn, can lead to brain damage or even death. It is therefore important for medical professionals to understand which treatment options are most effective following these kinds of injuries.
A team of neuroscientists from the University of Cambridge, decided to compare two treatment options to test their effectiveness. Using a sample of 400 traumatic injury patients from 20 countries over a 10 year period, patients were randomly assigned to one of two groups.
Patients in one group would undergo a craniectomy – a controversial type of surgery in which a portion of the skull is removed to allow a swelling brain room to expand. The patients in the second group were placed under medical management, which involved stabilizing the patient and preventing brain swelling by non-surgical means.
The researchers found that the risk of death for craniectomy patients was significantly reduced. Furthermore, a follow-up survey showed that the patients who survived following a craniectomy continued improving from six to 12 months after injury. As a result, after 12 months, around 45% of craniectomy patients reported being independent at home, compared with just 32% of medical management patients.
Peter Hutchinson, a neurosurgery professor at Cambridge, said: "Traumatic brain injury is an incredibly serious and life-threatening condition. From our study, we estimate that craniectomies can almost halve the risk of death for patients with a severe traumatic brain injury and significant swelling. Importantly, this is the first high-quality clinical trial in severe head injury to show a major difference in outcome. However, we need to be really conscious of the quality of life of patients following this operation which ranged from vegetative state through varying states of disability to good recovery."
Cambridge neuroscience lecturer, Angelos Kolias, added: "Doctors and families will need to be aware of the wide range of possible long-term outcomes when faced with the difficult decision as to whether to subject someone to what is a major operation. Our next step is to look in more detail at factors that predict outcome and at ways to reduce any potential adverse effects following surgery. We are planning to hold a consensus meeting in Cambridge next year to discuss these issues."
© Copyright IBTimes 2025. All rights reserved.





















