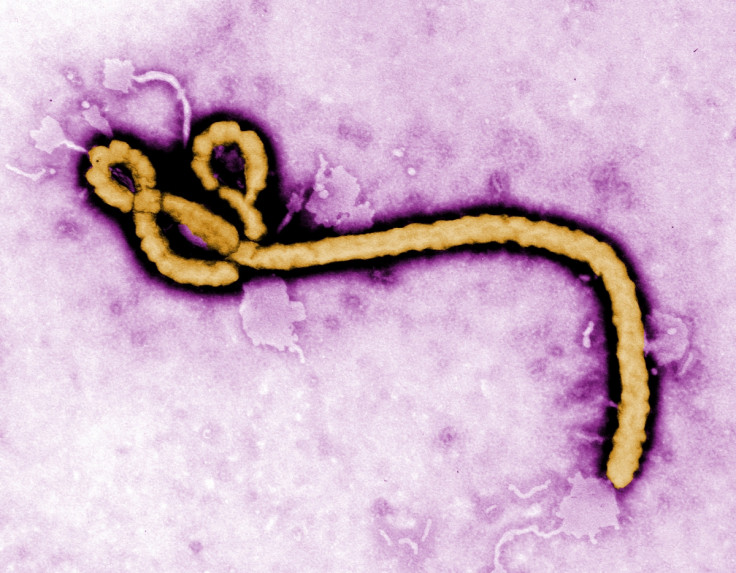
How Ebola adapted to better infect and kill humans during the last outbreak
The Ebola virus mutated early on in the epidemic to become more infectious to humans.
Mutations to the Ebola virus during the devastating epidemic of 2013-2016 may have increased its ability to infect humans. In two papers published on the same day, scientists suggest that the mutations reflect a human-specific adaptation of the virus, and may help explain why this recent outbreak was the worse seen to date.
Since the virus was discovered in 1976, Ebola virus disease (EVD) outbreaks have been controlled afterwards to at most a few hundred cases and have affected geographically limited areas. This has made the 2013-2016 epidemic even more shocking as nearly 30,000 people were infected over three years.
Multiple factors can explain why the outbreak in West Africa was particularly dramatic. Socio-economic factors, such as violent conflicts, poverty and the fact the authorities were slow to respond were problematic, but scientists have also wondered if unique genetic changes to the virus may not also have played a role.
"During the epidemic, a question remained: was there something different about the Ebola virus in this outbreak? High-profile computational model studies have tried to answer this by looking at the virus' genetic sequences", Jeremy Luban, author of one of the two studies, told IBTimes UK. "If you take all these papers, the general conclusion is there was nothing really different about this virus. However, these studies didn't experimentally test whether the mutations gave the virus a replication advantage".

More infectious and more deadly
The paper co-authored by Luban focuses on a mutation known as GP-A82V. Constructing evolutionary trees of the Ebola virus, the researchers showed that the mutation emerged very quickly in 2014, just before the number of cases increased exponentially. This new strain had a greater capacity to infect human cells than the original virus which had first circulated in Guinea. Clinical data obtained by the scientists suggest that it was also more deadly.
In the second paper, researchers also reconstructed the virus' family tree to identify mutations that could potentially signal adaptation to humans. They studied a number of mutations to the gene that encoded the Ebola virus glycoprotein – including the GP-A82V mutation – and infected bat and human cell lines.
The researchers observed that these mutations made the virus more infectious in humans but not in bats. This suggests that the mutations are indeed an adaptation to human hosts. "As the virus adapted to humans and became more infectious, infectivity in bats decreased. If they are the virus' natural host, it is unlikely we'll see the same mutations in bats. Now that the epidemic is controlled, we think these mutations have died out, but the question is whether they will appear again during potential future outbreaks", Jonathan Ball from the University of Nottingham, one of the authors of the second paper, told IBTimes UK.

Why these mutations had not been spotted in previous outbreaks is not clear yet. "Since past epidemics were a lot smaller in scale, it is possible that there had not been enough human-to-human transmissions for the mutations to arise. It's also possible that the small number of Ebola virus sequences available from these outbreaks meant they were difficult to spot"", Ball adds.
The results of the two studies could be important to manage future epidemics and find new therapeutic options. "The findings emphasise the importance of real-time monitoring. We don't know the significance of the mutation for dealing with future Ebola outbreaks but we know from other viruses such as HIV that this kind of information is crucial to decide what drug we should give people. It can also help us in the context of vaccination research", Luban says.
© Copyright IBTimes 2025. All rights reserved.






















