New study examines how serotonin leads to functional brain activity
A new study examines the effects of drugs that activate serotonin receptors on humans with cognitive deficiencies and mood disorders.
A recent study published in Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, examines the effects that serotonin-boosting drugs have on human adults with cognitive deficiencies, which can lead to mood disorders and other psychiatric conditions.
The study was published by Elsevier, a Dutch academic company that specialises in advancing the progress of scientific, medical and technical experiments performed by professional institutes.
Limited treatments for cognitive deficiencies currently exist (i.e. medication, reading books, memory training) but previous neuroscience studies in humans and animals have suggested that various drugs that activate serotonin receptors in the brain can reduce the debilitating symptoms. Despite these extensive studies, it remained unclear on the effects that serotonin-boosting medication, such as laxative prucalopride, has on brain activity.
Serotonin is a chemical that carries messages between nerve cells in the brain and throughout the body. This chemical plays a prominent role in rudimentary body functions such as mood, sleep, digestion, bone health, nausea, wound healing and sexual desire. Serotonin receptors in particular can be located in various parts of the brain, including the frontal lobe and hippocampus, and are known for regulating mood and mediating cognitive function; they also serve as the primary targets of antidepressant medications.
To conduct the study, researchers enlisted the help of fifty physically healthy volunteers. Half of the volunteers were prescribed a six-day course of prucalopride, a highly selective drug which binds itself to certain serotonin receptors, whilst the other half unknowingly received placebos. Throughout the project, the participants underwent scanning with functional magnetic resonance imaging along with resting state functional connectivity (rsFC), where the brain remains functionally and metabolically active.
Angharad de Cates, PhD, from the Department of Psychiatry at the University of Oxford and lead author of the study, commented on the study, saying: "Our previous studies on prucalopride demonstrated that even at low clinical doses it can improve cognition and memory in healthy volunteers. This latest research provides a neurological mechanism by which this might occur."
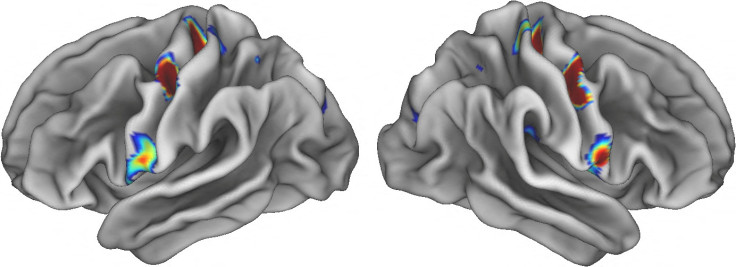
Researchers found that the participants who received prucalopride displayed more functional brain connectivity between major cognitive networks, including networks for processing thought and information processing, during their resting state.
For instance, there was more rsFC between regions of the anterior cingulate cortex and the lateral occipital cortex, a region that helps us pay attention to significant objects. Additionally, medicated participants compared to the placebo controls showed decreased rsFC in the default mode network, which is a brain network that is automatically activated during mind wandering.
Dr de Cates commented on these results, saying: "This provides further evidence that prucalopride is having an effect in areas of the brain that improve cognitive function, both by increasing and reducing connectivity between specific brain regions as required."
Associate Professor of Oxford University and joint senior author of the study, Susannah Murphy, PhD, also commented: "Appropriate connectivity between and within these brain networks is needed to think properly, and this connectivity has been shown to be abnormal in depression. Here, the participants taking prucalopride had better scores on cognitive tests the day of the scan compared to the placebo participants."
Dr Murphy concluded her thoughts on the study by stating that untreated cognitive deficiencies have a significant impact on the quality of life of people with depression, with the study providing further evidence that serotonin-boosting drugs are a "novel way" of treating depression and cognitive impairment.
© Copyright IBTimes 2025. All rights reserved.






















