Treating brain tumours with Zika virus destroys cancer cells
Virus was able to effectively target a type of cancer cell which is resistant to normal treatments.
The Zika virus, which is known to cause devastating damage to the brains of developing fetuses, may be an effective treatment for a deadly form of brain cancer. New research has found that the virus – an outbreak of which caused widespread fear in 2015 – kills a type of cancer cell that is particularly resistant to standard treatments.
The study shows that the virus can be harnessed to target malignant cells in the brain, improving the life chances of people suffering with glioblastoma – one of the most aggressive brain cancers, which kills most patients within a year of diagnosis.
"We showed that Zika virus can kill the kind of glioblastoma stem cells that tend to be resistant to current treatments and lead to death," said Michael S. Diamond, Professor of Medicine at Washington University School of Medicine and the study's co-lead author.
The team's findings were published in The Journal of Experimental Medicine
Normally, the disease is treated aggressively with surgery followed by chemotherapy. Despite this, most tumours recur within six months, often because a small number of the resistant glioblastoma stem cells survive, which simply cause a new tumour to grow once treatment has finished.
This ability of these glioblastoma stem cells to regenerate reminded researcher Zhe Zhu of a group of cells that are found in young, growing brains – known as neuroprogenitors. The Zika virus is known to target and destroy neuroprogenitors, which is why infected babies are often born with tiny, malformed heads.
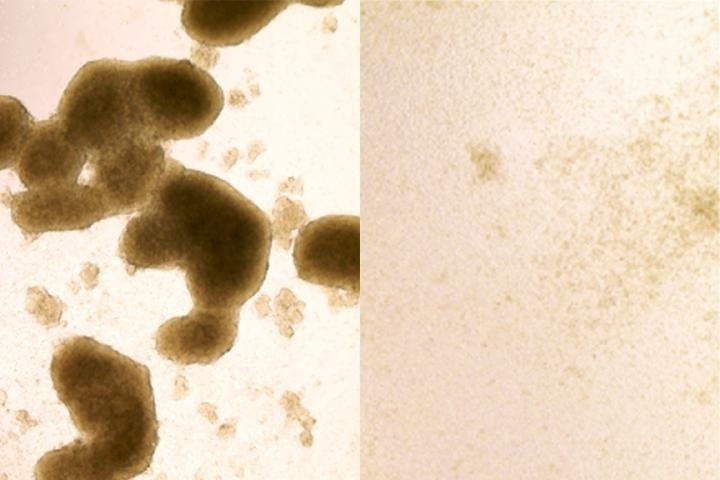
So, in collaboration with scientists from the Washington University School of Medicine and the University of California School of Medicine, he set up a study to determine whether Zika could be effective in destroying brain cancer stem cells. To test this, the team infected tumours that were removed from patients with two strains of the virus. Both strains spread through the tumours, killing the cancer stem cells, while largely avoiding other types of cells.
This suggested to the researchers that a treatment combining standard chemotherapy with Zika infection had complementary effects. The Zika virus targeted the regenerating stem cells and the chemotherapy destroyed the larger part of the tumour.
"We see Zika one day being used in combination with current therapies to eradicate the whole tumor," said Milan G. Chheda, a co-author of the study.
However, if it was to be used as a treatment, Zika would have to be injected directly into the brain. The virus cannot be introduced anywhere else in the body because the body's immune system will try to remove it before it reaches its target.
While injecting a virus known to cause brain damage directly into the brain seems like a worrying idea, in reality, it may be fairly safe. This is because Zika primarily targets neuroprogenitor cells that are rare in the adult brain, hence why infection in adults only causes mild symptoms. Foetal brains on the other hand are packed full of neuroprogenitors.
To confirm that the virus was safe to inject into the brain, researchers conducted tests to ensure it would not infect any non-cancerous cells. In addition, they introduced two mutations into the virus' genes that weakened its defences to a point where it would be eliminated quickly in healthy cells but could spread in tumour cells, which have a poor antiviral response.
"We're going to introduce additional mutations to sensitise the virus even more to the innate immune response and prevent the infection from spreading," said Diamond, who also is a professor of molecular microbiology, and of pathology and immunology. "Once we add a few more changes, I think it's going to be impossible for the virus to overcome them and cause disease."
© Copyright IBTimes 2025. All rights reserved.





















